Understanding Infection
How do infections spread?
Infectious agents may be spread to and from residents, employees, visitors, instruments, equipment, or the environment. The level of risk relates to the type of clinical contact healthcare workers have with potentially infected or colonised residents, instruments, or the environment, and the health status of the healthcare worker themselves (e.g., immunised or immunocompromised).
Chain of Infection
Transmission occurs when the infectious agent leaves its reservoir or host through a portal of exit, is conveyed by some means of transmission, and enters through an appropriate portal of entry to infect a susceptible host.
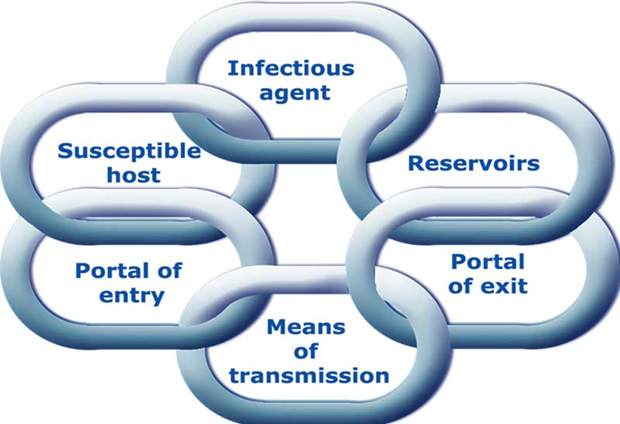
The reservoir of an infectious agent may be residents, employees, or visitors. This includes people with active diseases, people in the incubation period, or people colonised by the infectious agent but without the apparent disease (carriers).
Reservoirs may also include food, water, the environment, or vectors such as flies, mosquitoes, and ticks.
Routes of Transmission
Contact Transmission
This is the most common transmission mode and usually involves transmission by touch or via contact with blood or bodily substances. Contact may be direct or indirect.
Direct contact occurs when infectious agents are transferred from one person to another, for example, a resident's blood entering a healthcare worker's body through an unprotected cut in the skin.
Indirect contact involves the transfer of an infectious agent through a contaminated intermediate object or person, for example, a healthcare worker's hands transmitting infectious agents after touching an infected body site on one resident and not performing hand hygiene before touching another resident.
Examples
Multi-resistant organisms (MRO/MDROs)
Clostridioides difficile
Norovirus
Highly contagious skin infections/infestations (e.g., impetigo, scabies)
Droplet Transmission (Respiratory Transmission)
This can occur when an infected person coughs, sneezes, or talks during specific procedures. Droplets are infectious particles larger than 5 microns in size. Respiratory droplets transmit infection when they travel directly from the respiratory tract of the infected person to susceptible mucosal surfaces (nasal, conjunctivae, or oral) of another person, generally over short distances. The force of expulsion and gravity limits the droplet distribution and is usually at least 1 metre. However, droplets can also be transmitted indirectly to mucosal surfaces (e.g., via hands).
Examples
Influenza virus
Meningococcus
Rhinovirus
RSV
COVID-19
Airborne Transmission
This may occur via particles containing infectious agents that remain infective over time and distance. Small-particle aerosols are created primarily during breathing, talking, coughing, or sneezing, and secondarily by evaporating larger droplets in low-humidity conditions. Specific procedures such as airway suctioning and those that induce coughing can promote airborne transmission. Aerosols containing infectious agents can be dispersed over long distances by air currents (e.g., ventilation or air conditioning systems) and inhaled by susceptible individuals without contact with the infectious person. These tiny particles can transmit infection into small airways of the respiratory tract.
Examples
Measles (rubeola) virus
Chickenpox (varicella) virus
M. tuberculosis bacteria
The susceptible host
Resistance to pathogenic organisms varies greatly depending on the organism's virulence and the host's susceptibility. The most susceptible hosts include persons with diabetes, lymphoma, leukaemia, neoplasia, agranulocytosis or uraemia, and those treated with antibiotics and steroids. Age, chronic debilitating disease, shock, coma, and trauma (accidental or surgical) also influence susceptibility. Persons who have immuno-suppression because of chemotherapy, irradiation, or the presence of immuno-suppressive viruses such as HIV may also be particularly prone to infection.
Infection vs. colonisation
Exposure to an organism does not always lead to infection. In some individuals, colonisation occurs.
Colonisation is the multiplication of a micro-organism at a body site or sites (such as the skin, mouth, intestines, or airway) without eliciting an immune response or any evidence of infection. The individual does not become unwell and becomes a healthy carrier, although colonisation may sometimes lead to disease.
Infection is the successful transmission of a micro-organism to the host with subsequent multiplication, colonisation, and invasion of the bodily tissues. Infection results in a measurable immune response by the host.